Pediatric Urology
1) Hypospadias
Hypospadias refers to a wide range of anomalies, wherein the urinary opening is located at an abnormal position little proximal to the normal position. The incidence is approximately 1 in every 500 male infants.
The classic triad associated with hypospadias:
• Abnormally displaced urinary opening.
• Excess of dorsal prepucial skin (hooded prepuce) and deficiency of prepuce ventrally.
• Bending of the penis (chordee).
All these deformities may be present to various extent in a child.
CONCERNS:
My child has hypospadias. When should the treatment of my child begin?
The treatment of hypospadias is always surgical correction.
Except very minimal variants of hypospadias, which will never cause any functional compromise, and need treatment only for cosmesis, most varieties of hypospadias need surgical reconstruction.
The treatment may be single or multistaged.
The main criteria for repair is an adequate sized penis. Usually single stage correction is undertaken at around 1 year of age.
When multi-staged correction is planned, chordee correction is done at the first stage at around 7-8 months. Correction of chordee prevents the restriction of penile growth. Delay in correction of the chordee may restrict the penile length.
The most important relevant fact is that the excess prepucial skin in these babies is used to repair the urethral tube defect. Hence it is very essential to preserve this skin. We often see patients who have already been circumcised (ritual circumcision). It is very difficult to treat these patients. Kids with hypospadias should never be circumcised.
Whom do we consult for the treatment of my child?
Pediatric Surgeons, Pediatric Urologists, Plastic Surgeons are trained to treat these defects. But the concerned surgeon must be treating small babies routinely and the unit treating the baby must have adequate expertise in treating small babies.
What are the results of surgical treatment?
15 years back, complications after hypospadias repair were fairly common. Common complications after surgery were fistula formation (passage of urine from multiple places), stricture (narrowing of the newly formed passage), wound infection, bleeding, and complete wound dehiscence. But in the last decade, there has been a lot of advancement in the surgical techniques, surgical suture material, operative.
magnification and instruments for handling delicate tissues without damaging them. Now the complications are few and far between. But even the best center in the world dedicated to only hypospadias repair cannot boast of a complication free outcome. The fistula rate following hypospadias repair is now around 5% in the best hands. Our complication rates match that of the best centres in the world.
What is the problem if I do not treat my child?
In glanular, coronal and some very distal penile hypospadias variants, there should not be any functional problems throughout the life of the child. The entire concern is cosmetic. Peer criticism, criticism from his spouse form important issues for concern. But all said and done, parents run the risk of being criticized by the child when he grows up as the treatment options with reasonable outcome are now available in the city. This was not the scenario 10-15 years back.
For all the other variants of the disease, treatment is a must for the following reasons:
• Narrow meatus may lead to bladder outflow obstruction.
• Proximal location of the penis may hamper the delivery of the sperm in the vaginal vault.
• Bending of the penis may lead to painful erection and difficulty in coitus.
What investigations should be done and when?
Ultrasonography should be done as soon as possible after the diagnosis of the ailment to rule out associated anomalies in the urogenital system
2) Chordee
A Chordee is a congenital anomalous condition of the male penis wherein the penis is curved ventrally. This is due to abnormal development of the penile tissues. It may or may not be associated with an abnormally opening of the urethra (Hypospadias).
This ailment commonly goes unnoticed if it is not associated with hypospadias and is known during adolescence when the boy undergoes a painful erection.
The only effective treatment of chordee is through surgery. The surgery is pretty straightforward and it should ideally be done before the age of 2 years. The patient can usually be discharged 48 hours after the surgical correction. During this period a catheter is used to drain the urine from the bladder.
A minor chordee usually gets corrected by itself.




3) Vesicoureteral Reflux : Role of Deflux
Vesicoureteral reflux (VUR) is the retrograde or backflow of urine from the urinary bladder into the ureter and ultimately towards the kidneys.
Normally there is a high pressure zone at the urterovesical junctions which prevents this backflow. When this valve action is lost, VUR results.
VUR can be primary or secondary. In primary cases, due to developmental anomaly of the kidneys and the ureters, there is laxity of the ureterovesical junction. In secondary cases, VUR results from rise in the pressure inside the urinary bladder. This may be due to urinary outflow obstruction or some disease of the spinal cord or other reasons leading to high bladder pressure.
In this article, we are dealing with the management of primary VUR.
How can we diagnose VUR?
VUR can be diagnosed by a radiological examination called MICTURATING CYSTOURETHROGRAM (MCUG).There is a belief among the parent population that MCUG is extremely painful and distressful and morbid for the baby or the child. But if done under the supervision of a Pediatric surgeon and a Pediatric Nephrologist, it is truly painless and morbidity free. Another concern is radiation exposure. Nowadays we do it under fluoroscopic control and try to minimize the radiation as much as possible.
MANAGEMENT OPTIONS :
A) MEDICAL:
Since the reflux is a developmental anomaly, and the resultant damage in the kidney has been there from birth, we often treat the baby or the child with long term low dose antibiotics to prevent any urinary tract infection as it is believed that renal damage occurs only when infected urine goes back and hammers the kidneys.
Problems with medical treatment:
• Non compliance – Many parents particularly from low socio-economic background often do not continue regular dose of antibiotics.
• Cost – The antibiotic prophylaxis has to be continued for often 5 -6 years, and this involves a huge cost.
• Resistance – Since a single antibiotic is continued for a long period of time, it often gives rise to resistance. So when any child on prohylaxis develops a febrile UTI, it is often resistant to all oral medications.
• Ongoing Reflux continues to damage the kidneys and often when scars develop on the DMSA scans, it is often irreversible.
B) SURGICAL:
This is the time tested traditional treatment for infants and children with VUR. There are many surgical options and all procedures have a success rate of > 90%.
Problems with traditional surgical treatment:
• Major procedure: Antireflux surgery is a major procedure involving a long in-house admission. The standard post operative pain is significant. There are a few catheters dangling from all around. The urine remains reddish for around 7-10 days. The complete recovery takes almost a month and often longer.
• Cost: Since the hospital stay is 7-14 days, any surgical procedure entails a huge cost.
• The urinary bladder needs to be split open for a reimplantation (intra-vesical). Often a growing urinary bladder when cut open and resutured, may cause scarring and may restrict the bladder growth. Hence it is advised not to go for reimplantation at a very tender age.
How recent advances in surgery have surpassed some of these problems?
Laparoscopic , Robotic and Vesicoscopic ureteral reimplantation have surpassed most of the problems of traditional surgery stated above. There is no incision on the abdomen or the bladder. The hematuria subsides much early (within 48hours usually) and hence the sole urinary catheter often can be removed within 48hours and the child recovers very fast and is back to normal life by a week. The pain is also much much lower.
C) DEFLUX:
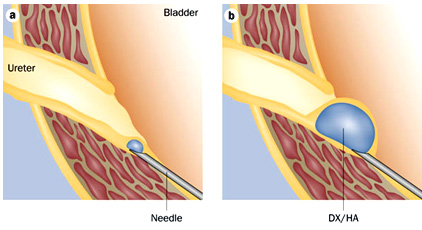
Deflux is the trade name for Dextranomer microspheres. It consists of 2 types of sugar based molecules (polysaccharides) , dextranomer and hyaluronic acid of non animal origin. It is an implant which is stable long term, remains in position and does not disappear over time . It is injected around the ureteral opening to create a mound that stops urinary reflux. Over time, the gel combines with fibroblasts and collagen, which stabilize the position and the size of the implant.
This is a short procedure, completely non-invasive, requires 10-15 minutes and requires a very short anesthesia and without intubation. It can be done as a daycare procedure. The child can return to normal life from the next day.
The antibiotic prophylaxis can be stopped within a month.
Our protocol is to do a repeat Ultrasonography after 3 months and repeat MCU after 5 months. If necessary a second or sometimes a third injection may be needed.
VUR and PREGNANCY
It has been shown that girls with unilateral or bilateral VURs who have been treated without surgery and continue to have VURs have increased propensity to develop pyelonephritis during their pregnancy.
A simple non-invasive DEFLUX injection has the potential to cure the reflux forever.
PATIENT INFORMATION FOR DEFLUX PROCEDURE
Know About Deflux?
What is a Deflux implant procedure?
Deflux is a sterile, biodegradable gel used to treat vesicoureteral reflux (VUR). The Deflux implant is injected into the bladder wall where the ureter enters the bladder, forming a bulge at the opening. The bulge reduces the size of the opening, to prevent urine from flowing backwards into the ureter. The opening is still flexible so urine can flow into the bladder, as it should. Deflux is gradually replaced by the body’s own tissue, so the bulge remains. General anesthesia is given. Then the surgeon inserts a cystoscope, a thin viewing device, into the bladder through the urethra (where the urine comes out), and injects the Deflux. The procedure usually takes less than 30 minutes.
How does Deflux work?
The hyaluronic acid in Deflux is a chemical that naturally occurs and breaks down in the body. The dextranomer in Deflux remains and is slowly replaced by the body's own tissues, forming a little bulge. The bulge makes it harder for the urine to flow back up the ureter and to the kidney. The bulge is permanent and corrects the reflux.
Who can have this procedure?
Based on the success rates, this procedure is recommended for children with grade II, grade III, and possibly grade IV reflux. The treatment should not be used in patients who have:
• Two kidneys that don't work at all
• An abnormal pouch in the bladder wall
• An extra ureter (the tube that carries urine from the kidney to the bladder)
• Active urinary tract infection
• Active voiding dysfunction, or abnormal emptying of bladder
What happens on the day of the procedure?
Preparation for the procedure takes about an hour, and the procedure itself takes about 30 minutes. Your child will be put to sleep with a general anesthetic for the procedure. You can be with your child as he or she recovers.
Since there are no abdominal incisions made for this procedure, your child can go home the same day.
What happens during the procedure?
Once child is asleep under general anaesthetic, the cystoscope is lubricated, inserted into the urethra and passed up into the bladder. Sterile saline is then pumped through the cystoscope to expand the bladder and allow clear view of the inside of the bladder. Deflux is then injected and the telescope is removed.
Will my child feel any pain?
Child may feel uncomfortable after the procedure – 1 in 20 patients get pain in the loin on the side of the Deflux injection which may last up to 24hours.
What happens after the procedure?
Child will usually go home on the same day following the procedure. As general anaesthetia will be given , you will need to arrange for someone to stay with your child for 24 hours after the procedure.
What do I need to do after I go home?
There are no special precautions associated with Deflux that you need to take after the injection. A three-day course of antibiotics is given to take home – it is important to complete the course.
How effective is Deflux ?
Deflux procedure is effective not only in eliminating VUR on radiologic studies, but also in reducing the incidence of UTIs and antibiotic use in children with VUR.
What are the risks for the procedure?
Bruising and swelling – Child may have some bruising and swelling around your urethra from the cystoscope being inserted. This should clear up after a few days.
Bleeding – Some patients may find that their urine is slightly pink for a few days after this procedure. Drinking plenty of water (about three litres spaced out over 24 hours) can help to clear your urine.
Infection – Child may develop a urine infection after cystoscopy, which could result in a fever (raised temperature) and painful urination. Drinking plenty of water after the procedure can reduce the risk of infection. Oral antibiotics after the procedure to help to reduce this risk further.
How successful is this procedure?
Treatment with Deflux has a higher success rate for those with lower grades of reflux. One study reported a 95 percent success rate for grade II reflux, 71 percent success rate for grade III and 43 percent success rate for grade IV reflux. Similarly, a second study reported an 87 percent success rate for grade II reflux, a 75 percent success rate for grade III and 41 percent success rate for grade IV reflux. In another study, researchers reported a 78 percent success rate for both grades II and III reflux, and 66 percent success rate for grade IV reflux.
The success of the procedure is also dependent on the individual child and the doctor's technique. Sometimes more than one treatment is needed to build up a bulge large enough to reduce the child's reflux.
4) Balanoposthitis
What is this condition called?
This is commonly mistakenly diagnosed as paraphimosis. This condition usually results from insect bite. There is severe swelling of prepuce which settles with conservative treatment and hardly ever requires surgery.

5) Epispadias
This picture shows Epispadias with Minimal Exstrophy Bladder.


A Large Hydrocele in a 6 years Child - These Cases Need Two Incisions :
One Inguinal for Herniotomy and a Scrotal Incision for Eversion of Sac

Testicular Torsion in a Young Child. Needed Removal of Left Testis. Lesson : If There is Any Redness / Painful Scrotum, Immediately Consult Pediatric Surgeon. Any Torsion Beyond 24 Hours Usually Needs Excision of Testis.


Epispadias defect where the Baby Passes Urine through an Opening on the Upper Surface of The Penis. Can be fully corrected surgically.

This 8 months Female Baby was straining to pass Urine and was repeatedly complaining of Lower Abdominal Pain for 3 months. Pediatrician treated her with all possible Medicines and USG was done which was normal. Nobody examined the Genitalia which was fused living a very small opening for the Passage of Urine. This is called LABIAL SYNECHIAE. This is Physiological Adhesion caused due to deficiency of the Hormone Estrogen. Can be treated with Manual Separation and Local Ointments.

6) Pyeloplasty

Traditional Incision for Pyeloplasty Surgery (Surgery to Remove Blockage of the Urinary Pipe near the Kidney). Even now Many Surgeons make such a Large Incision.
7) True Paraphimosis
True Paraphimosis. Usually can be Reduced at The Clinic. Sometimes need Circumcision Later on.

8) Ectopic Testis

This is a Congenital Condition where the Testis Descends from the Abdomen and Stays at an Abnormal Location. Usual Abnormal sites are Lower Abdomen, Upper Thigh, Perineum, Root of the Penis and Femoral Canal. Usually these Testes, Unlike Undescended Testes have relatively normal Function and can almost always be placed in the Scrotum.
9) Testicular Torsion

Testicular torsion is a cause of complete necrosis/ destruction of testis which is to a great extent treatable surgically if presents in golden hour (upto 4 hours of onset of torsion).
When to suspect torsion?
Sudden enlargement of one side of the scrotum with severe pain and often associated with redness. The child may also have pain in the ipsilateral groin or even lower abdomen. Often it is associated with nausea and vomiting.
Common age groups?
In the newborn period and in adolescent age group
How to confirm the diagnosis?
Ultrasonography with colour Doppler study shows no vascularity in the affected testis. But often it is missed on ultrasound. So if the doctor suspects that the baby/ child is suffering from torsion of the testis, there is no harm in exploring the scrotum under general anesthesia, especially in the districts and periphery where proper round the clock facilities for USG is not available. The good thing about exploration is that once detwisted and fixed, often the vascularity returns back and there is minimal, if any long term damage to the testis.





