Counselling for Neonatal Disease
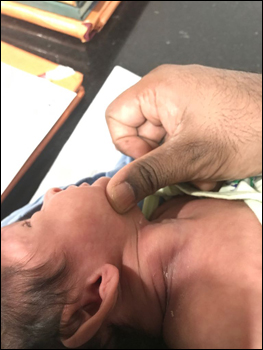
Right sided Sternomastoid Tumor (Torticollis). There is a Swelling in the Neck usually seen after Birth. The Baby mostly looks towards the Opposite Side. It usually responds to Physiotherapy. Rarely needs Surgical Correction.
Neonatal Intestinal Obstruction
When to suspect?
A newborn has abdominal distension, vomits out greenish liquid (bile) or milk immediately after feeds, does not pass or passes scanty black stool (meconium). He/ she may become lethargic. One may see moving sausage shaped lumps in the abdomen (visible peristalsis).
What are the ailments which lead to intestinal obstruction in a newborn baby?
• There may be complete non development of a part of our intestinal tract, in which case the baby shall not be passing meconium at all or may pass whitish mucus (Intestinal Atresias).
• There may be obstruction at the outlet of the stomach (Pyloric Stenosis).
• There may be compression from outside at various areas of the gastro-intestinal tract (Malrotation / Band Obstruction).
• The baby may have a non functioning or malfunctioning lower G.I tract (Anorectal Malformation / Hirschsprungs’ Disease / Anal Stenosis)

What is the management of such situations?
• In all the situations mentioned above, a Pediatric Surgical consultation is a must. Most of these ailments can be completely cured by a competent Pediatric surgeon unless there are already irreversible complications.
Are contrast studies Harmful for Newborns?
• In adults, barium studies are a common diagnostic tool to diagnose the site of intestinal obstruction.
• But in babies, a contrast study (a series of x-rays) involves too much exposure to radiation. CT scan involves even greater degree of radiation.
• If at all required, we do a Contrast Screening under Fluoroscopic Guidance, which involves a much lesser amount of radiation.

Isn’t a major surgery too risky for a newborn?
• A newborn with an intestinal obstruction is already in a very critical state and all the parameters are already compromised.
• Surgery, in the hands of an experienced team, carries minimal morbidity. An experienced team includes an experienced Pediatric surgeon, an experienced anesthesiologist, an experienced team of properly trained nursing staff to care for newborns and a proper Neonatal Intensive Care Unit.
What are the recent advances in the management of a newborn with intestinal obstruction?
Parenteral nutrition: Nowadays in babies with necrotizing enterocolitis and other ailments where a portion of the alimentary tract is damaged, we put in a long line and administer total parenteral nutrition which has improved the outcome of neonatal intestinal obstruction babies to a great extent.


A Newborn with Huge Abdominal Distension
Early intervention makes a difference
Preterm baby delivered at 32 weeks with premature rupture of membranes and polyhydramnios (excess maternal amniotic fluid) developed abdominal distension from birth.
The baby was managed at a peripheral district hospital for 5 days before referring to us.
First x ray shows hugely distended loops of gut with no rectal gas shadow.
After starting Perioheral nutrition and orogastric decompression, the x ray still shows distended proximal intestinal loops.
Surgical findings: malrotation with volvulus, leading to midgut volvulus before birth and hence loss of significant part of small intestine. Only 3 cm of terminal ileum was present and 39 cam of duodenum and dilated proximal jejunum.
In this situation often there is intestinal failure known as “short bowel syndrome”.
They do not tolerate full feeding by mouth and may need prolong parenteral (by IV drip) nutrition.
The more premature the baby it is more likely that the intestine which could be preserved will subsequently grow in length thus resulting in a greater capacity for adaptation.
35 cm of neonatal small bowel is associated with a 50% probability of weaning from parenteral nutrition. Presence of ileocecal valve has historically been considered a favourable prognostic factor.
Serum citrus lime measurement gives us a rough idea whether we can wean the baby from PN. Persistent Serum Citrulline level < 12 micromoles/L are usually not wearable.